AORTIC dissection is a potentially life-threatening emergency. The condition arises due to a tear in the inner lining of the aorta, which may allow blood to flow into a false channel in the aortic wall. The enlargement of this false lumen can compress the true lumen and restrict blood supply to the vital organs. Alternatively, the false lumen may rupture.
There are many classification systems for aortic dissection, but the most useful is the Stanford classification, which classifies dissections into those originating in the ascending aorta (Type A) and those in the descending thoracic aorta (Type B).
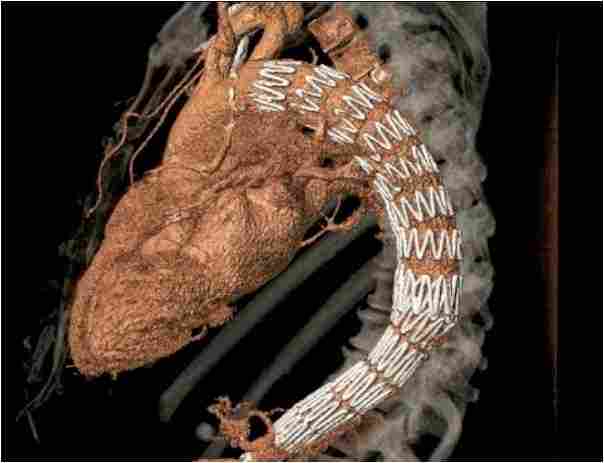
Type B aortic dissections require intervention when they are complicated by rupture, imminent rupture or malperfusion. Surgery historically was associated with a mortality of 30%. Despite the relative infancy of thoracic endografting, these procedures are now routinely used in the treatment of Type B aortic. The early results of endovascular treatment of acute complicated Type B dissections are reasonably well characterised and suggest a substantial early mortality advantage over open surgical treatment.
A recent report from the US in patient sample has identified a considerable mortality advantage over conventional surgical repair. Less certain is the place of endovascular therapy for chronic Type B dissections or in lesions that may be classified as sub-acute (between two and six weeks after the onset of dissection). There is a relatively sparse literature reporting the outcomes of endovascular therapy in non-acute dissections.

There has been a debate concerning the development of new grafts specifically focused on dissection. These lesions have different characteristics to thoracic aneurysms, for which the majority of grafts were designed. Specifically-designed grafts might have less radial force, increased conformability and be less rigid than current endografts. Similarly, there has been considerable interest in bare metal stents that aim to facilitate the aortic remodeling which accompanies placement of an endograft. Contemporary research studies will define the place of these materials in clinical practice.
Despite these difficulties, endovascular development may offer a therapeutic modality for cases of surgically untreatable Type A dissection
At present, Type A dissections are treated with emergency cardiac surgery, which has an excellent success rate but a mortality of 20% and a turn down rate of up to 40%. Several pathologies may be candidates for endovascular treatment including isolated ascending aortic aneurysms, cannulation site false aneurysms and some Type A dissections. The anatomical and physiological challenges to endovascular therapy of the ascending aorta remain formidable and include:
- Proximal fixation close to the aortic valve and coronary ostia
- Distal fixation which may impinge on the innominate artery
- Curvature of the distal ascending aorta
- Sizing discrepancies in pathological conditions
- Haemodynamic forces in this arterial segment
- Potential for fatal retrograde dissection
Despite these difficulties, endovascular development may offer a therapeutic modality for cases of surgically untreatable Type A dissection. Selective studies have demonstrated that up to 30% of patients with Type A dissection are unable to undergo surgical treatment. The mortality in these cases is high, and endovascular therapy may be a possible alternative. Approximately 50% of Type A dissections occur 2cm or more distal to the coronary ostia and these patients might derive some benefit from coverage of the primary entry tear, and proof of concept studies are now in progress.




