With so many advancements in healthcare happening right before our eyes – we speak to the experts about emerging technologies and how new innovations have the potential to transform the way the UK public will receive healthcare and alleviate some of the huge strain felt by the NHS
The evolution of healthcare is underway.
New technology is being introduced all the time, alongside bold scientific discoveries that are taking modern medicine to whole new levels.
And, with so many advancements, it pays to keep a finger on the pulse and be informed as to what might come next.
With this in mind, X-ray protection and radiology supplier, Rothband, predicts the emerging technologies that have the potential to transform how the UK public receive healthcare, and talks to the manufacturers about how they will help.
1. From the comfort of your own home:
More services are expected to be delivered in the community or in patients’ own homes. One of the companies delivering these services is JimJam, a firm that offers online physiotherapy sessions through remote assessments.Chief executive, Chris Kennelly, says: “Teleconferencing or video call is here already, is growing in its scale and scope of service use, and has a lot of interest, both inside and outside the NHS.
How it’s affecting healthcare now is largely around speed and convenience for patients and clinicians.
“For example, our patients want to be able to see a physio at a time and place that suits them, so being able to see one today, from their own home or office and to not have to travel is great. If you then extend this scenario to people living or working in remote geographical locations, the impact is far greater.”
If more people are having remote assessments, then the NHS needs less infrastructure. That means smaller and fewer buildings, which has a financial and environmental impact, not to mention the reduced carbon impact of all those patients not having to drive to appointments anymore
Longer term, JimJam hopes to alleviate some of the huge strain felt by the NHS.
“The potential future impact is much, much bigger,” said Kennelly.
“If more people are having remote assessments, then the NHS needs less infrastructure. That means smaller and fewer buildings, which has a financial and environmental impact, not to mention the reduced carbon impact of all those patients not having to drive to appointments anymore.“Clinical capacity also increases because clinicians aren’t travelling as much, meaning more time for clinical function.”
He concludes: “While I’m hugely enthusiastic about the prospects of video call technology within healthcare, we must also be realistic.
“This will not replace same-room consultations entirely and we will always need this, but video call technology offers us a way of better utilising precious clinical resources and, not just through reducing costs, but also improving access and quality at the same time. We’re some way off this, but it does look like It is achievable - and quickly.”
As patients become more informed, the technology moves in tandem.
video call technology offers us a way of better utilising precious clinical resources and, not just through reducing costs, but also improving access and quality at the same time. We’re some way off this, but it does look like It is achievable - and quickly
Commenting on the digitalisation of healthcare is Joe Bloom, entrepreneur and founder of online wellbeing start-up Mentovo.
“In this modern age individuals are not only more educated about their own health, but are inquisitive about their own wellbeing.
Giving the public the tools to manage their own wellbeing is going to be a priority of future healthcare systems.
“Standards are changing as some public health systems transition into digital systems to allow for this, but are very slow on the uptake with private practices appearing to offer a more-tailored service.”
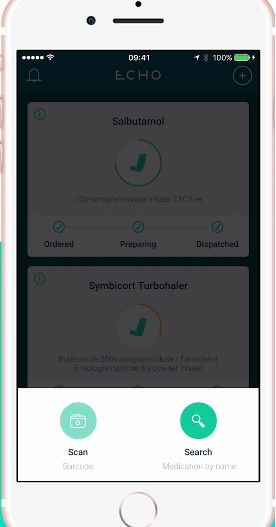
Echo helps with medicine adherence
2. Your smartphone isn’t just for selfies
Rothband spoke to Stephen Bourke from London-based Echo, an EU start-up company which is producing devices to improving medicine adherence.
Bourke said: “My co-founder and I both take medication for long-term conditions and felt that the process of ordering repeat prescriptions every two months to be fragmented, confusing and a chore. So, on a blank piece of paper, we mapped out what the ideal service should look like. Then we built it.
“The problem Echo solved is medication adherence.
Between a third and half of all meds aren’t taken as directed. Our goal is to maximise possession and nudge patients towards better compliance, using affordable and ubiquitous smartphone technology
Between a third and half of all meds aren’t taken as directed. Our goal is to maximise possession and nudge patients towards better compliance, using affordable and ubiquitous smartphone technology. This will reduce waste with respect to GP appointments and medication, and improve outcomes in the long run.”
And so, Echo was born.
An app that came directly from personal experience, it is now supported by NHS professionals and is a must-have app for those who find repeat prescriptions laborious.
Bourke adds: “We have had some fantastic support from GPs, pharmacists and nurses, as well as people within NHS digital and BSA.
“We have NHS clinicians on the team, which is important when it comes to navigating a complex system.”
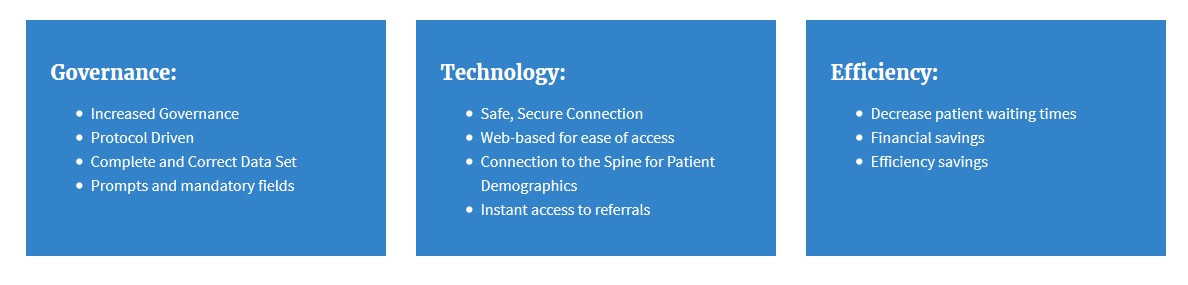
Casper is an easier referral system for radiotherapy patients
3. Easier referral for radiotherapy patients
Cievert aims to make the referral process as convenient as possible for patients undergoing cancer treatment, providing online referral platforms to 15% of radiotherapy departments with a project named ‘Casper’.
It offers a secure, intuitive, web-based referral platform allowing clinicians to refer their patients from any NHS clinic in the country. Referrals are immediate, secure and adhere to locally-defined clinical pathways to ensure consistency.
Commenting on the background of Cievert is business development manager, David Birchmore.
He said: “Radiotherapy is a complex clinical pathway that requires input from multiple staff groups to deliver the patient through to treatment.
“With a traditional paper system, this is a linear pathway; so the last person in the process is not alerted to the patient until everyone else has actioned their own work.
At Cievert, we see the future of technology as empowering the patient to better self-manage health complaints while at the same time facilitating rapid access to expert healthcare when required
“With Casper, once the form is submitted it is available instantly for any staff member to work on in parallel, thus having a huge impact on waiting times.
“One of our customers decreased the time of their referral pathway by 13 days with the help of Casper.”
He added: “At Cievert, we see the future of technology as empowering the patient to better self-manage health complaints while at the same time facilitating rapid access to expert healthcare when required.
“Too often, patients are followed up routinely because the technology and infrastructure is not in place to support and monitor the patient remotely.
“If it were we would be seeing patients followed up at the time and place that is most appropriate, rather than ‘in six weeks in outpatients’.
“There will also always be a requirement to make processes more efficient and cost effective”.
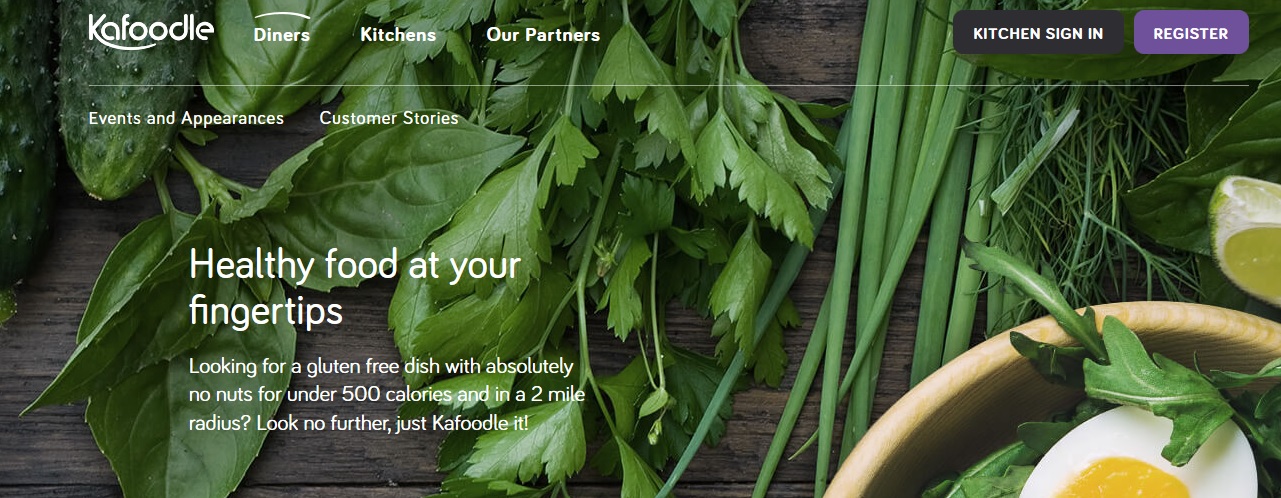
Kafoodle Care is a cloud-based personal nutrition care plan
4. Fine-tuning your food experience – making hospitals more hospitable
If you’re not too fond of hospital food, this bit of technology is for you.
Kafoodle Care is a cloud-based personal nutrition care plan designed for use in hospitals, care homes and schools.
It takes note of all allergies, as well as nutritional and medical needs to offer a tailored service to patients.
Co-founder, Tarryn Gorre, said: “The idea for Kafoodle Kare came from witnessing first-hand how poorly hospitals were catering to patients with specific dietary needs – whether it be diabetes, a food allergy or a personal preference.
“Some patients, especially children, spend substantial amounts of time in hospital and there seemed a clear opportunity to make their experience with food while in care a better one.
This, with growing government legislation around food, gave us the idea of Kafoodle Kare.
“Patient care plans are supposed to monitor nutrition and dietary intakes. However, even electronic care plans rely on visual cross checking to spot allergic and medical reactions.
Food intolerances are rarely catered for, meals lack nutrition and taste, and there is no quality standard benchmarked across healthcare providers.”
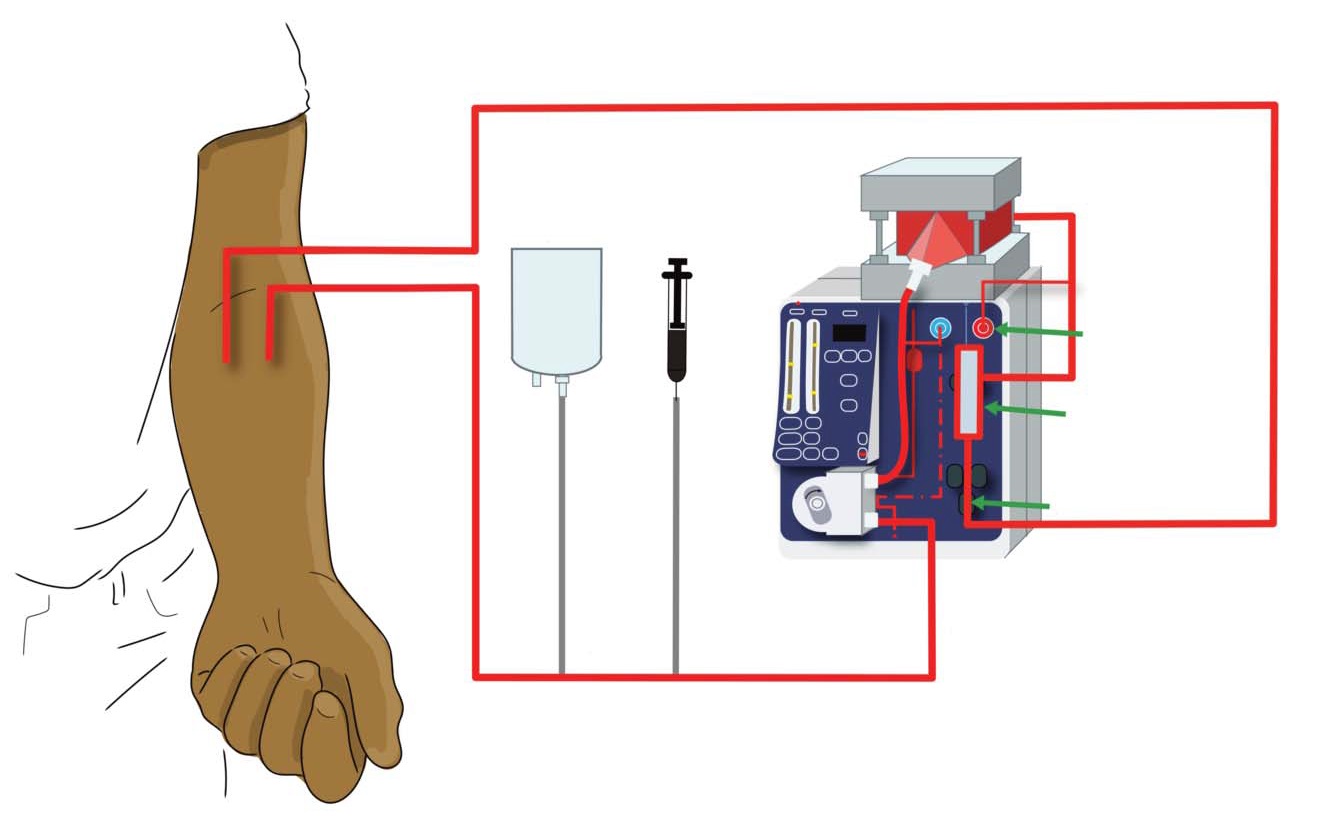
The MediSieve Filter is set to offer a new lifeline for malaria patients
5. Blood filtration system to combat malaria
Dr George Frodsham is the man behing MediSieve – a response to problems with existing malaria treatments.
“Typically, treatments for blood-borne diseases are pharmaceutical drugs that aim to kill the disease-causing pathogens.
Across a range of diseases, these drugs frequently have a number of problems. They are non-specific, and target ‘good’ things as well as ‘bad things’; they can cause severe side-effects, sometimes even fatal; they are expensive, and they are slow acting.
“MediSieve’s approach is to remove the pathogens, rather than killing them,” said Frodsham. In this way, even when the MediSieve Filter is used alongside drugs, many of the problems of drugs are alleviated.
Using Medisieve, pathogens are eliminated much faster; there are no side-effects; it doesn’t harm healthy blood components; and it can remove things that drugs cannot target.
In the long-term, our technology could be used to treat a huge range of different diseases affecting patients all around the world
“Our ambition is to provide a new tool to enable doctors to remove practically anything directly from the bloodstream,” said Frobisher.
“In the long-term, that could mean that our technology could be used to treat a huge range of different diseases affecting patients all around the world.”
Overall, these are exciting times, not only for tech, but in terms of what it can bring to healthcare.
The solutions here span a broad range, yet they all look to transform how care is offered, and how it is received.
Here’s to the future…




