ARPA-H's ImagiNg Data EXchange (INDEX) programme and the Digital Pathology Association Regulatory and Standards Task Force (DPA R&STF) have provided a comprehensive framework for digital development in pathology, while recognising that pathology infrastructure challenges continue to significantly undermine AI efforts.
But are they partly to blame for the lack of progress?
Pathology is often lumped together with the other diagnostic disciplines, admonished for not keeping pace. But this perspective is fundamentally flawed.
Trying to drag pathology down the same path as radiology and cardiology threatens not only to hinder the effective implementation of digital pathology, but also risks jeopardising its ability to address its critical infrastructure problems.
A unique starting point
Pathology’s unique infrastructure demands a singular approach.
1. A different medium: Whole Slide Images (WSI) not digital images
Pathology's reliance on glass slides since the 1800s sets it apart from cardiology and radiology. This key difference means pathology faces a much longer road to digitalisation and a greater number of hurdles to overcome.
2. Image size and number: A higher information density
The size of the images used in pathology is also significantly larger. The exact file size will vary by resolution and modality, but if a high-resolution pathology image is 80 times larger than a radiology image, it's clear why the gap between needed and existing IT infrastructure is so vast.
Whole Slide Images (WSIs) also need to be stained and, depending on the technique performed, a single WSI may require up to 10 separate stainings to gain sufficient insights for diagnosis. This means even larger datasets per patient:
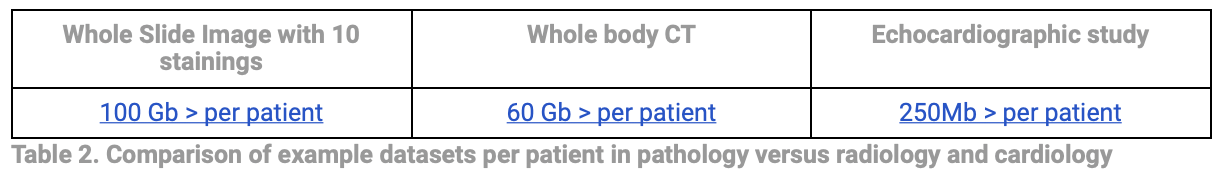
This higher information density presents significant challenges for storage, transfer, and computational analysis in digital pathology workflows.
3. Pathologists' workflows are unique: LIS versus RIS
Changing pathology systems and infrastructure profoundly alters how pathologists work, impacting everything from lab organisation and sample tracking to collaboration, meaning new processes need to be built from the ground up. This shift is more profound for pathology than for any other diagnostic discipline. Consider, for example, the differing workflows of pathologists and radiologists.
Pathology’s Laboratory Information Systems (LIS) serve as a central hub, allowing pathologists to manage the entire lifecycle of lab specimens, integrate instruments, automate workflows, and ensure accurate result verification. In contrast, while Radiology Information Systems (RIS) handle workflow and reports, it's the Picture Archiving and Communication System (PACS) that stores, retrieves, and facilitates the viewing of images.
