Strategies designed to reduce pressure on GP resources need to be accelerated if the NHS is to safeguard the workforce and the patients they serve.
Primary care networks (PCNs) play a fundamental role in meeting the goals of the NHS Long Term Plan and £2.4billion has been committed by the Government to fund primary care across the country by 2023/24 under the Network Contract Directed Enhanced Service (DES) Contract Specification 2020/21.
This includes funding for larger PCN care teams across a wide range of health professionals, including clinical pharmacists, physician associates, first contact physiotherapists, community paramedics, and social prescribing link workers; allowing GPs to focus more on patients with complex needs.
And, increasingly, the importance of community teams is being recognised: working across neighbourhood or place level they can deliver integrated health and social care across a wider community to provide tailored care for patients.
For a PCN or ICS in England, the priority for any change must be to improve service delivery while also reducing pressure on frontline staff
This model has been working successfully in Scotland and Wales for several years.
NHS Tayside has such an integrated care model firmly embedded across three regions and 63 GP practices.
Since its inception, the model has managed over 400,000 patient contacts, half of the patients’ appointments having been created by their GP practice, illustrating how this has helped relieve pressure on overstretched GPs and direct patients to more-appropriate services.
In contrast, despite the funding and commitment, progress within England remains patchy, with just a handful of ICSs grasping the opportunity.
So, what is holding back essential progress in delivering integrated services across primary care?
Empowering clinicians
One of the biggest barriers to change is the legacy technology that prevents effective clinician access to information.
At NHS Tayside, the entire model is predicated on rapid, secure access to patient records from multiple practices, supported by data-sharing agreements.
Every healthcare professional has access to up-to-date patient information, including medical history and medications and the Electronic Health Record (EHR) is also updated automatically following every patient interaction.
With a shared appointment facility for each service across locations, irrespective of GP practice, patients have wider access to services – and the ability to opt for the most-suitable time and place for the interaction.
With many PCNs and ICSs having a mix of EHR solutions in place – which do not share information – the evolution of integrated services in England has floundered
However, with many PCNs and ICSs having a mix of EHR solutions in place – which do not share information – the evolution of integrated services in England has floundered.
Without immediate access to patient information from any location, and every patient interaction quickly available within each and every EHR, the model will not realise the full benefits.
The resulting duplicate recording, and clinicians using multiple systems, is a further step away from the single, consistent EHR that is key to realising the goals of a patient-centric health service.
For a PCN or ICS in England, the priority for any change must be to improve service delivery while also reducing pressure on frontline staff.
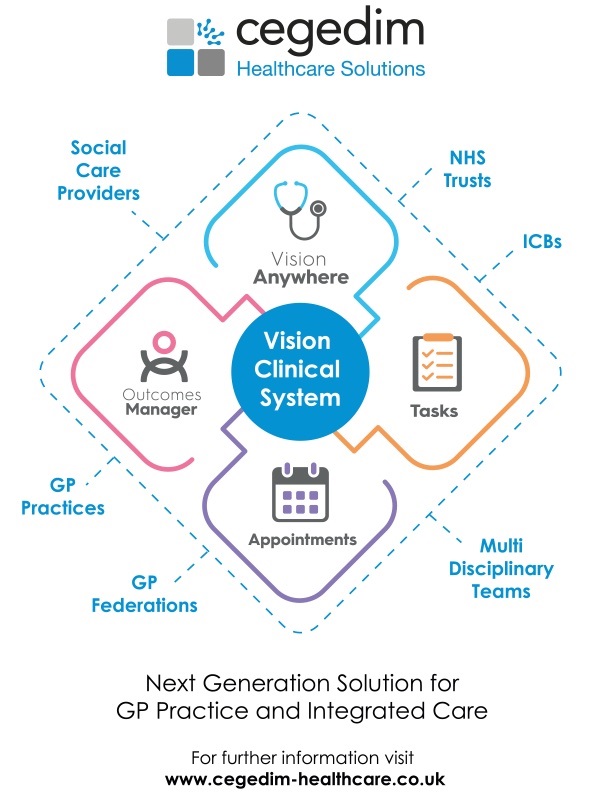
As such, it is vital that any integrated care solution allows clinical teams to support multiple practices from a single system while ensuring the primary care EHR is maintained in as near-to-real-time as practical.
An integrated model for the future
It is not practical, or necessary, to consolidate onto a single EHR within a PCN or ICS – especially given the likelihood of further geographic changes to NHS structure.
What is needed is a solution that integrates seamlessly with existing EHRs to provide the single patient view, preferably in an intuitive manner.
With powerful integration, the NHS can eradicate many of the technology compatibility barriers and progress towards realising the benefits of an integrated care vision through fast access to patient information and ease of appointment booking for both patients and clinicians.
This will require an ever-greater degree of provider collaboration to ensure services co-design new, effective care models in which clinicians and patients can quickly access the information and resources they need
In addition, by providing broader system access to patient information, this integrated approach allows more-granular analysis of the population health data to enable a population health management approach to segment groups with similar characteristics and stratify into levels of need to redesign services to better meet those needs.
This will enable the intelligence-driven evolution of primary care.
It will highlight opportunities to reconfigure the workforce to achieve further reduction in GPs’ workload by diverting cases which can be managed by other professionals, leaving GPs’ expertise to manage the complex cases and rationalising GP specialist care, for example, clinicians with specialist interests in dermatology; diabetes; MSK, across a PCN or place footprint.
The cumulative data from this can then be used across an ICS to identify cohorts of patients to help to determine whole system priorities.
A collaborative appoach
There is some way to go in England before such a vision is adopted – and key to achieving this shift must be an increase in the range and number of services integrating across a footprint.
The neighbourhood approach is key, as underlined in the recent Fuller Report, which recommends greater integration of the NHS into social and community care at the PCN/neighbourhood level.
This will require an ever-greater degree of provider collaboration to ensure services co-design new, effective care models in which clinicians and patients can quickly access the information and resources they need.
It will require technology companies willing and committed to partnering with the NHS to deliver real change
The broader the reach, the more accurate and complete will be the population health information these models are based upon - and the greater the insights to enable PCNs and ICSs to understand how best to evolve care and manage workloads to support both clinicians and patients in the optimal way moving forward.
And it will require technology companies willing and committed to partnering with the NHS to deliver real change.
Providing appropriate levels of ‘write and read’ access to a single, shared care record solution is just part of the evolution. From the integration of community-based multi-disciplinary teams (MDTs), primary care, and specialists to share information to support the work of virtual wards, to system-wide management of long-term conditions such as diabetes and COPD across primary, secondary, and community teams, primary care systems must be a core component of a far-wider, patient-centric vision of holistic care. Without that, the valuable and unique role of primary care in the new vision of integrated care will never be realised.
